The condition of the esophagus plays a significant role in maintaining health. Chronic inflammation in this area can result in a range of uncomfortable symptoms and may indicate more serious underlying health problems.
This condition is frequently associated with gastroesophageal reflux disease (GERD), a disorder wherein stomach acid backs up into the esophagus, causing irritation and inflammation.
Consequently, patients often report symptoms such as dysphagia (difficulty swallowing) and chest pain.
Early recognition of these symptoms is essential for effective management and for lowering the risk of serious complications, including the possible advancement to Barrett’s esophagus and esophageal cancer.
‘Click here to learn more about:’ the ultimate anti inflammatory guide
Understanding Esophageal Inflammation
Esophageal inflammation can arise from a variety of sources, often leading to chronic irritation. The underlying causes include conditions like gastroesophageal reflux disease (GERD), where gastric acid damages the lining of the esophagus.
Symptoms associated with this condition encompass:.
- Dysphagia
- Chest pain
- Irritation in the throat
- Heartburn
Little-known consequences related to chronic inflammation include an elevated risk of metaplasia, which requires close monitoring. Persistent inflammation may signal broader systemic issues that could lead to severe health conditions. Addressing these aspects effectively is important for ongoing health management and treatment success.
Chronic Inflammation Solutions for Squamous Mucosa Symptoms
Chronic inflammation in the squamous mucosa can produce discomfort and a variety of symptoms. Addressing these issues necessitates a targeted approach that incorporates:
- Dietary changes, focusing on anti-inflammatory foods such as omega-3 fatty acids, antioxidants, and fiber-rich items.
- Lifestyle modifications, including regular exercise and stress management techniques.
- Potential medical interventions, which could involve topical treatments or medications for more severe symptoms.
Regular consultations with healthcare professionals can enhance management strategies and ensure that any persistent or worsening symptoms are monitored closely. Maintaining hydration and ensuring adequate sleep are crucial components of overall inflammation management.
Proactive management of chronic inflammation can significantly improve health outcomes.
For effective results, consider the following:.
- Engage in regular physical activity.
- Practice stress reduction techniques such as yoga or meditation.
- Avoid processed foods and trans fats to help lower inflammation levels.
- Consult with healthcare providers for personalized treatment plans.
- Stay committed to routine check-ups to monitor inflammation and associated symptoms.
Biopsy Techniques For Esophageal Issues
Accurate diagnosis of esophageal disorders is paramount for effective treatment. Endoscopic biopsy stands out as a pivotal method, allowing physicians to obtain tissue samples directly from the esophagus.
Advanced techniques, particularly endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA), enhance diagnostic accuracy by improving the specificity of biopsies.
Challenges in sample collection arise frequently, especially in patients with inflammation or motility issues.
Precise training and technique are essential to avoid complications during these procedures. Addressing the complexities of obtaining a biopsy is important for ensuring a reliable pathology report and guiding subsequent patient management.
Challenges in Sample Collection
Obtaining high-quality biopsy samples can be obstructed by various factors.
Examples of these challenges include:
- Presence of inflammation in the esophagus, which can make tissue acquisition difficult.
- Patients with motility issues may present additional difficulties during sampling.
- Technical proficiency is crucial to minimize the risk of complications, including bleeding or perforation.
Thus, effective training is vital for clinicians performing these biopsies.
The Link Between Acid Reflux And Esophagitis
Establishing the connection between acid reflux and esophagitis sheds light on esophageal health. Gastroesophageal reflux disease (GERD) frequently leads to stomach acid irritating the lining of the esophagus, generating significant inflammation. Chronic exposure to acid can create long-lasting changes in the squamous mucosa, leading to conditions like Barrett’s esophagus. Metaplasia may occur as the body adapts to repeated injury, emphasizing the complexity of this process. Untreated esophagitis can escalate into serious complications, necessitating effective management strategies and regular monitoring to mitigate risks associated with chronic inflammation and potential cancer progression.
Long-Term Effects of Acid Reflux
Chronic acid exposure can have several implications for esophageal health. Notable effects include:
- Development of Barrett’s esophagus, a condition that increases the risk of esophageal cancer.
- Increased risk of esophagitis, characterized by pain and discomfort.
- Potential for strictures or narrowing of the esophagus due to persistent inflammation.
Management of these conditions is vital to promote healing and prevent further complications.
Chronic Inflammation Solutions for Squamous Mucosa Symptoms
Chronic inflammation in the squamous mucosa can lead to discomfort and various symptoms. Addressing these symptoms requires a focused approach:
- Dietary changes: Incorporating anti-inflammatory foods, such as omega-3 fatty acids and antioxidants, is beneficial.
- Lifestyle modifications: Regular exercise and stress management techniques can significantly contribute to reducing overall body inflammation.
- Medical interventions: Consultation may be necessary for severe symptoms; treatments could involve topical applications or medications.
- Regular monitoring: Follow-up with healthcare practitioners can enhance management strategies and ensure improved health outcomes.
Esophageal Health
- Approximately 20% of adults in the United States experience symptoms of gastroesophageal reflux disease (GERD).
- Barrett’s esophagus occurs in about 5-10% of patients with chronic GERD, significantly increasing the risk of esophageal cancer.
- Chronic inflammation of the esophagus can lead to strictures, affecting 10-20% of patients with long-standing acid reflux.
- Dietary changes, such as reducing caffeine and fatty foods, can alleviate symptoms of esophagitis in many patients.
Identifying Signs Of Barrett’s Esophagus
Barrett’s esophagus is marked by alterations in the lining of the esophagus due to chronic irritation, frequently stemming from gastroesophageal reflux disease (GERD). Recognizing early signs is essential for effective management.
Symptoms can vary; notable signs include:.
- Dysphagia—difficulty swallowing, which may not always be apparent but can signify underlying conditions.
- Chronic heartburn that is resistant to antacids can indicate more serious issues.
- Regurgitation of food or liquids may also serve as a warning signal.
- Unexplained chest pain, particularly during meals, warrants further investigation.
Early detection and timely intervention can significantly enhance treatment outcomes and mitigate the risk of esophageal cancer.
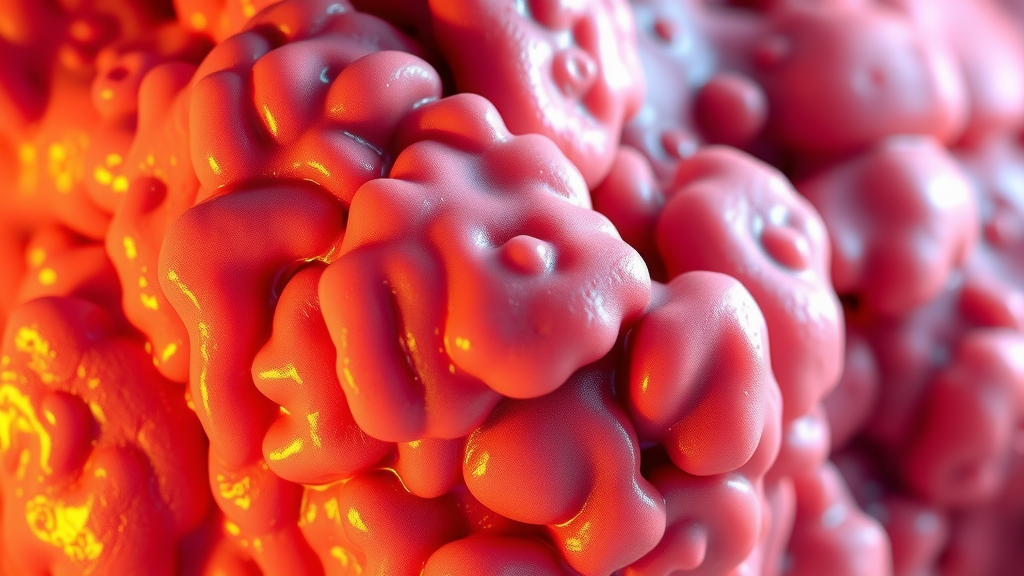
Exploring Reactive Changes In Esophageal Tissue
Chronic irritation leads to reactive changes in the esophageal tissue, presenting a significant concern in conditions like Barrett’s esophagus. These alterations can include:
- Chronic inflammation that prompts shifts within the squamous mucosa, often resulting in metaplasia, where normal cells adopt columnar characteristics.
- Biopsies are crucial in identifying underlying pathology, as they reveal reactive or reflux changes.
- Specific inflammatory markers found in biopsy samples can reflect the extent of irritation.
Monitoring these changes through regular screenings and endoscopies is fundamental for effective management. Addressing chronic inflammation in squamous mucosa is essential for alleviating symptoms and improving overall health.
Chronic Inflammation Solutions for Squamous Mucosa Symptoms
Chronic inflammation in the squamous mucosa can lead to discomfort. Addressing this requires a comprehensive approach involving:.
- Dietary adjustments—Incorporating anti-inflammatory foods such as omega-3 fatty acids, antioxidants, and fiber-rich items can promote healing.
- Regular exercise—Physical activity contributes to reducing overall body inflammation.
- Stress management techniques—Practices such as meditation and yoga can mitigate inflammation levels.
- Medical consultation—For severe symptoms, healthcare providers may prescribe topical applications or medications.
Regular follow-ups with healthcare practitioners can enhance management strategies and improve quality of life.
Barrett’s Esophagus
- Approximately 10% of individuals with chronic GERD may develop Barrett’s esophagus.
- Regular endoscopies can detect precancerous changes in the esophagus early, improving treatment outcomes.
- Dietary modifications can significantly reduce symptoms and inflammation associated with esophageal disorders.
- Studies indicate that lifestyle changes, including weight loss and smoking cessation, can lower the risk of esophageal cancer in patients with Barrett’s esophagus.
Impact Of Gastroesophageal Reflux Disease On Health
Gastroesophageal reflux disease (GERD) presents significant health implications that extend beyond the esophagus. This chronic condition can lead to various systemic health issues due to persistent inflammation.
Complications triggered by GERD may include:
- Respiratory conditions: Chronic cough and asthma may result from acid aspirating into the airways.
- Dental erosion: Stomach acid can damage tooth enamel, leading to cavities and sensitivity.
- Esophageal adenocarcinoma: Studies indicate that untreated GERD increases the risk of this serious cancer due to changes in the squamous mucosa.
Lifestyle factors, particularly obesity and poor dietary choices, may exacerbate the effects of GERD. Several strategies can be considered to mitigate symptoms:.
- Dietary modifications: Incorporating anti-inflammatory foods can aid in reducing discomfort.
- Weight management: Losing excess weight is beneficial, as it may relieve pressure on the lower esophageal sphincter.
- Regular exercise: Physical activity is important for maintaining a healthy weight and reducing inflammation.
Addressing these interconnections is essential for developing effective management strategies aimed at improving overall health outcomes.
Role Of Endoscopy In Esophageal Pathology
Endoscopy is integral in assessing and diagnosing conditions related to GERD and its associated inflammation. This technological advancement has enhanced the ability to detect and treat esophageal issues effectively. Key advancements in endoscopic techniques include:
High-Definition Imaging
With sophisticated imaging capabilities, healthcare providers can clearly visualize the lining of the esophagus, allowing for a thorough assessment of potential damage.
Biopsy Sampling
During endoscopic procedures, biopsy sampling provides critical information through the evaluation of squamous mucosa. This process aids in identifying conditions such as:
- Metaplasia: A change in the type of cells lining the esophagus.
- Reactive changes: Alterations due to prolonged exposure to gastric acid.
Such advancements facilitate early detection and timely medical interventions. Regular follow-up with healthcare practitioners ensures comprehensive management of esophageal pathology and associated symptoms.
Chronic Inflammation Solutions for Squamous Mucosa Symptoms
Chronic inflammation within the squamous mucosa can lead to significant discomfort and various symptoms. Addressing these issues requires a focused approach, incorporating dietary changes, lifestyle modifications, and potential medical interventions.
- Dietary Adjustments: Consider incorporating anti-inflammatory foods such as omega-3 fatty acids, antioxidants, and fiber-rich options.
- Supplements: Natural anti-inflammatory supplements may be beneficial when integrated into daily routines.
- Exercise: Regular physical activity is crucial for lowering overall body inflammation.
Managing stress effectively can also contribute to reducing inflammation levels. Techniques such as meditation and yoga are recommended practices.
Medical Consultations
For persistent or severe symptoms, consulting healthcare providers is essential. Treatments may involve:.
- Topical applications to alleviate localized discomfort.
- Medications aimed at controlling inflammation.
Regular monitoring and follow-up visits can enhance management strategies tailored to individual needs.
Gastroesophageal Reflux Disease (GERD)
- Approximately 20% of the U. S. population experiences GERD symptoms regularly.
- Long-term GERD can increase the risk of esophageal adenocarcinoma by as much as 30 times.
- Weight loss of just 5-10% can significantly alleviate GERD symptoms in overweight individuals.
- Endoscopy is considered the gold standard for diagnosing esophageal conditions related to GERD.
Diagnosing Risks Associated With Esophageal Cancer
Identifying risks associated with esophageal cancer is imperative for early intervention. Various factors contribute to this risk, including gastroesophageal reflux disease (GERD), which can lead to significant changes in the esophagus, elevating the potential for cancer development.
Chronic irritation caused by gastric acid negatively impacts the lining of the esophagus, potentially resulting in precancerous conditions such as Barrett’s esophagus.
Critical Risk Factors
- Smoking: A history of smoking greatly increases risk, influencing cellular changes within the squamous lining of the esophagus.
- Genetics: Family history can indicate inherited mutations that enhance individual susceptibility to esophageal cancer.
- Obesity: Excess weight raises intra-abdominal pressure, contributing to GERD and subsequent risks.
- Alcohol Consumption: Regular intake of alcohol has been linked to an increased risk of esophageal cancer.
Continuous monitoring through endoscopy and biopsy is essential for early detection and management of these risk factors.
The Importance Of Mucous Membranes In The Esophagus
The protective roles of mucous membranes are fundamental to esophageal health. These membranes act as barriers against irritants and pathogens, thereby preserving the overall integrity of the esophagus. The mucus secreted serves to lubricate food passage, minimizing friction during ingestion.
Implications of Damage on Overall Health
- Esophagitis: Damage to mucous membranes can lead to esophagitis, which heightens the risk of further complications, including cancer.
- Chronic Inflammation: Ongoing inflammation may result in metaplasia, wherein normal squamous cells transform into columnar cells, increasing cancer risk.
- Management Strategies: Regular evaluation and monitoring of mucosal linings are essential to maintain their health and functionality.
To effectively address chronic inflammation and its symptoms, consider implementing dietary changes, lifestyle modifications, and potential medical interventions.
Chronic Inflammation Solutions for Squamous Mucosa Symptoms
Chronic inflammation can lead to discomfort and various symptoms. Solutions for managing inflammation include:.
- Dietary Adjustments: Incorporating anti-inflammatory foods such as omega-3 fatty acids and antioxidants is beneficial.
- Exercise: Regular physical activity can significantly reduce overall body inflammation.
- Stress Management: Techniques like meditation and yoga can help alleviate stress, which may exacerbate inflammation.
- Medical Consultation: Seek advice for severe or persistent symptoms; treatments could involve topical interventions or medications.
- Regular Monitoring: Follow-up appointments with healthcare practitioners can enhance inflammation management strategies.
It is crucial to adopt holistic approaches such as staying hydrated, getting adequate sleep, and avoiding processed foods to support healing and reduce inflammation.
Esophageal Cancer Risks
- Studies show that individuals with GERD have a significantly higher likelihood of developing esophageal cancer.
- Research indicates that smokers are up to three times more likely to develop esophageal cancer compared to non-smokers.
- Obesity is associated with a 50% increase in the risk of esophageal adenocarcinoma.
- Regular endoscopic screenings can detect precancerous conditions early, improving treatment outcomes.
Management Strategies For Esophageal Irritation
Addressing chronic inflammation of the esophagus involves employing a variety of strategies tailored to the individual’s needs. Pharmacological interventions, such as proton pump inhibitors (PPIs), play a significant role in reducing gastric acid production and alleviating symptoms associated with gastroesophageal reflux disease (GERD).
Alongside medication, lifestyle modifications are essential; adopting a diet that minimizes irritants—such as caffeine, spicy foods, and acidic items—can provide considerable relief.
Incorporating herbal remedies, including chamomile tea, has been noted for its soothing properties on the esophageal lining.
Additionally, stress management techniques, such as yoga and mindfulness practices, can enhance overall well-being. A combination of these methods creates a comprehensive management plan for individuals experiencing esophageal irritation.
Chronic inflammation can lead to discomfort affecting the squamous mucosa. Solutions for managing inflammation in this region include dietary adjustments, the use of anti-inflammatory supplements, and the adoption of healthier lifestyle practices.
Regular exercise coupled with stress management techniques is critical in reducing inflammation.
In some cases, medical consultation is necessary for persistent symptoms, with treatments potentially involving topical applications or specific medications.
Continuous monitoring and follow-up with healthcare practitioners support effective management strategies.
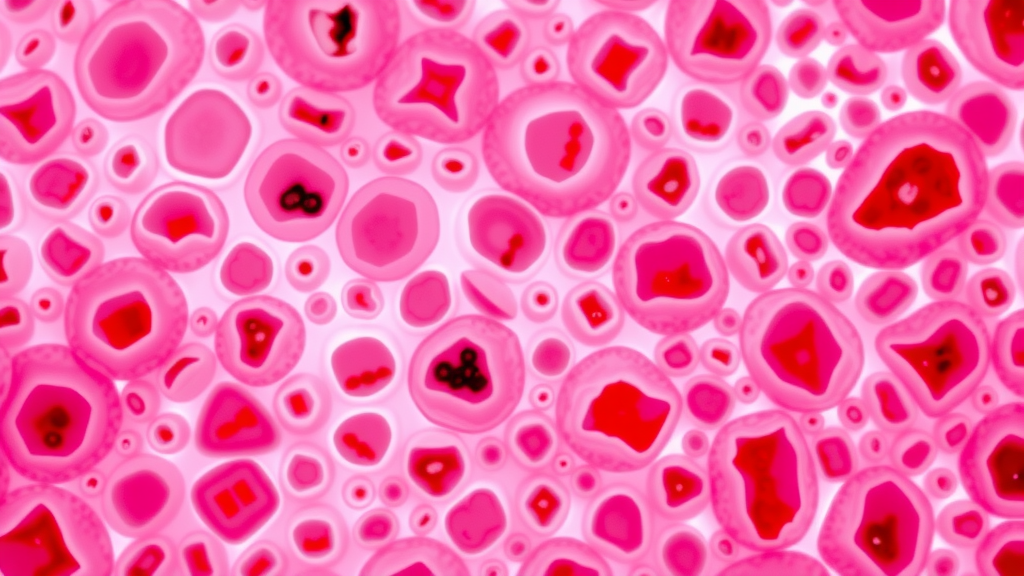
Understanding The Role Of White Blood Cells In Inflammation
The immune response is key in addressing esophageal conditions, particularly chronic inflammation.
White blood cells (WBCs) serve distinct roles during this process:
- Neutrophils: These are among the first responders to infection within the esophagus, initiating the inflammatory response.
- Lymphocytes: T-cells are involved in long-term immune responses, playing a critical role in chronic inflammation associated with conditions like Barrett’s esophagus.
- Eosinophils: These cells indicate allergic reactions and contribute to inflammation, especially in cases such as eosinophilic esophagitis.
- Monocytes: Transforming into macrophages, they clean debris and aid in healing the esophageal lining.
Recognizing these functions of WBCs can assist in guiding targeted treatments and improving patient outcomes for individuals facing various esophageal conditions. It is vital to consider the unique contributions of each type of white blood cell in forming effective management strategies for esophageal irritation and inflammation.
Esophageal Irritation Management
- Proton pump inhibitors (PPIs) can reduce gastric acid production, providing relief from symptoms associated with gastroesophageal reflux disease (GERD).
- Dietary modifications that limit irritants like caffeine and spicy foods can significantly alleviate esophageal discomfort.
- Regular exercise and stress management techniques, such as yoga and mindfulness, are crucial in reducing chronic inflammation in the esophagus.
- White blood cells, including neutrophils and lymphocytes, play essential roles in the immune response and chronic inflammation related to esophageal conditions.
Chronic Inflammation In Stomach | Unseen Triggers Behind Gastritis Symptoms
Chronic Inflammation Stress | Unseen Toll