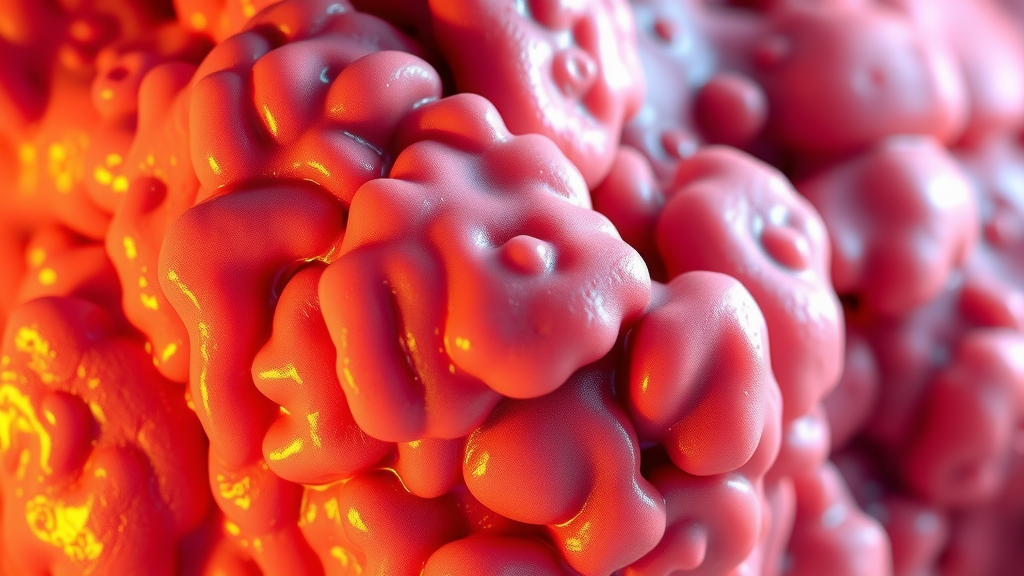
Chronic inflammation serves as a hidden driver of numerous health complications. Persistent inflammation can lead to mechanisms of fibrosis, where ongoing tissue damage may result in scarring.
Over time, the immune system becomes dysregulated, producing excessive inflammatory mediators that contribute to fibrotic disease.
Insight into these cellular and molecular mechanisms is essential for developing effective treatment strategies aimed at reducing inflammation.
By uncovering these unique insights, conditions such as autoimmune diseases and chronic respiratory disorders can be better addressed, ultimately paving the way for improved health outcomes.
‘Click here to learn more about:’ the ultimate anti inflammatory guide
Understanding Chronic Inflammation
Chronic inflammation manifests as a prolonged inflammatory response linked to various health issues. Often stemming from lifestyle and environmental factors, this condition has a substantial impact on health.
Common sources include:.
- Poor diet choices such as high sugar and processed food intake, leading to heightened inflammatory responses.
- Environmental influences like pollution that can aggravate the immune system, resulting in persistent inflammatory states.
Key inflammatory markers, such as C-Reactive Protein (CRP) and interleukins, serve as indicators of the body’s inflammatory status. Monitoring these markers contributes significantly to addressing the long-term effects of chronic inflammation on overall health.
Chronic inflammation can lead to serious diseases like arthritis, heart disease, and diabetes.
Implementing solutions for chronic inflammation can significantly improve symptoms. Consider the following recommendations:.
- Lifestyle modifications: Diet and exercise can effectively reduce inflammation levels.
- Anti-inflammatory diets: Focus on whole foods rich in antioxidants and omega-3 fatty acids.
- Regular physical activity: Aids in managing weight and reducing inflammatory markers in the body.
- Stress management techniques: Meditation, yoga, and deep breathing exercises contribute to decreased inflammation.
- Supplements: Curcumin, omega-3 fish oil, and probiotics may support anti-inflammatory pathways.
- Avoiding triggers: Processed foods, excessive alcohol, and smoking can mitigate symptoms.
- Adequate sleep: Crucial for the body’s healing processes and inflammation regulation.
- Integrative approaches: Combining conventional and alternative medicine can enhance treatment efficacy.
- Hydration: Plays a vital role in maintaining cellular health and reducing inflammation.
- Regular health check-ups: Monitor inflammatory markers and underlying conditions.
Addressing chronic inflammation is essential for restoring health and preventing further deterioration. Personalized approaches based on an individual’s health profile are critical for effective treatment. Educating oneself on inflammation and its effects can empower individuals to make necessary lifestyle changes and seek professional guidance from knowledgeable healthcare providers.

Unraveling Fibrosis Mechanisms
Fibrosis represents a complex pathological process marked by chronic inflammation, which leads to excessive connective tissue formation. This development is associated with several biological processes that initiate tissue scarring.
Various types of fibrosis arise from distinct conditions, including pulmonary fibrosis, liver fibrosis, and cardiac fibrosis, each impacting multiple organs.
Fibroblasts are essential in this process as they synthesize collagen, a primary component of the extracellular matrix.
The growth factor TGF-β serves as a significant mediator in the mechanism of fibrosis, promoting further collagen deposition and cellular proliferation. These cellular and molecular mechanisms are essential for developing targeted therapies against fibrotic diseases.
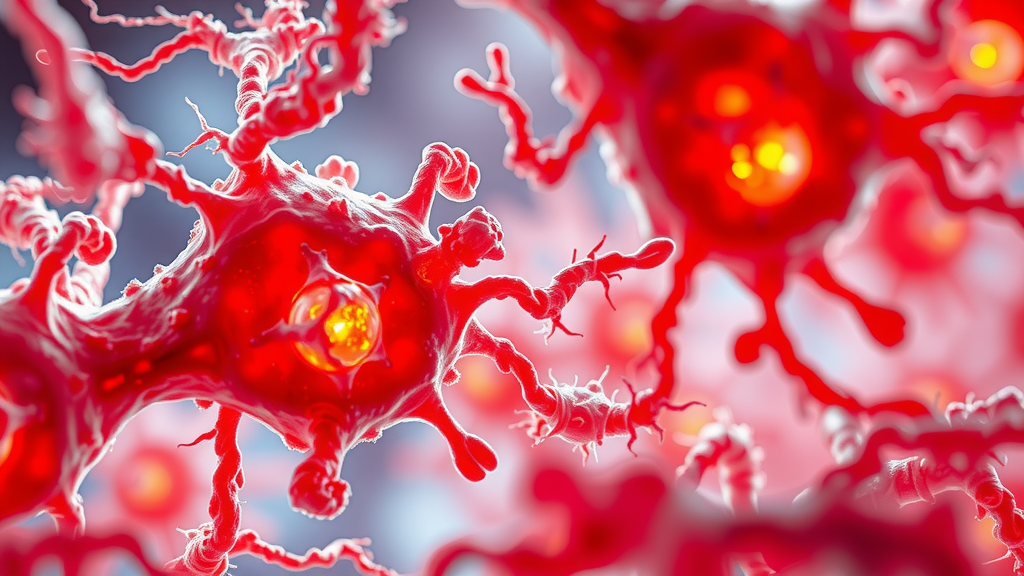
The Role Of Immune Cells
Immune cells play a vital role in chronic inflammation and the development of fibrosis, influencing both inflammatory responses and tissue repair mechanisms.
Macrophages and T cells are among the key players, with macrophages exhibiting diverse phenotypes that can either exacerbate or alleviate inflammation. These immune cells release various cytokines that can promote fibrosis by activating fibroblasts.
The balance of pro-inflammatory and anti-inflammatory signals is critical; in chronic conditions, macrophages often transition toward a pro-fibrotic phenotype, driving tissue remodeling and fibrosis.
A deeper understanding of these immune interactions holds promise for innovative therapeutic interventions against fibrotic diseases.
Strategies for Managing Chronic Inflammation
Effectively managing chronic inflammation is crucial for those experiencing its symptoms.
Several lifestyle modifications can significantly reduce inflammation:.
- Anti-inflammatory Diet: Incorporate whole foods rich in antioxidants and omega-3 fatty acids.
- Regular Physical Activity: Engage in exercise to manage weight and lower inflammatory markers.
- Stress Management: Utilize techniques like meditation, yoga, and deep breathing exercises to decrease inflammation.
- Health Supplements: Curcumin, omega-3 fish oil, and probiotics may support anti-inflammatory pathways.
- Avoid Known Triggers: Limit processed foods, excessive alcohol, and smoking to mitigate symptoms.
- Restorative Sleep: Ensure adequate sleep to support the body’s healing processes.
- Integrative Approaches: Combining conventional and alternative medicine can enhance treatment efficacy.
- Hydration: Maintain proper hydration to aid cellular health and reduce inflammation.
- Regular Health Check-ups: Monitor inflammatory markers and underlying conditions.
Long-term Implications of Chronic Inflammation
Chronic inflammation can lead to significant health issues, including diseases such as arthritis, heart disease, and diabetes. Persistent inflammation has the potential to cause irreversible tissue damage and fibrosis. Awareness of diet is critical; high sugar and refined carbohydrates can exacerbate inflammation, whereas foods like leafy greens, berries, nuts, and fatty fish are beneficial. Regular monitoring of markers such as CRP (C-reactive protein) can indicate levels of inflammation in the body. Environmental factors, hormonal imbalances, and personalized approaches based on individual health profiles are also important considerations for effective management.
Fibrosis and Inflammation
- Fibrosis can develop in various organs, including the lungs, liver, and heart, significantly affecting overall health.
- Macrophages can adopt different phenotypes, influencing inflammation levels and the progression of fibrosis.
- A diet rich in antioxidants and omega-3 fatty acids can help mitigate chronic inflammation and its effects.
- Monitoring inflammatory markers like CRP can provide insights into the body’s inflammatory status and guide treatment strategies.
Impact Of Cytokines On Fibrosis
Cytokines significantly influence the complex dynamics of fibrosis development in the body. One prominent cytokine, Transforming Growth Factor-beta (TGF-β), is recognized as a pro-fibrotic agent that promotes fibroblast proliferation and facilitates the conversion of fibroblasts into myofibroblasts.
These myofibroblasts are responsible for secreting surplus collagen, which leads to the deposition of extracellular matrix components typically associated with various fibrotic diseases.
Conversely, the Interleukin-10 (IL-10) cytokine functions as an anti-inflammatory mediator, playing a protective role by inhibiting the signaling pathways of TGF-β, thereby reducing fibrotic activity.
Understanding these contrasting roles of cytokines offers insights into therapeutic strategies aimed at restoring balance in inflammation and fibrosis.
Key cytokines involved in fibrosis include:.
- TGF-β: Promotes matrix deposition and myofibroblast formation.
- IL Reduces inflammation and fibrotic signaling.
- Interleukin-1 (IL-1): Encourages inflammatory pathways that can lead to fibrotic changes.
- Platelet-Derived Growth Factor (PDGF): Stimulates fibroblast proliferation and migration.
Recognizing this dichotomy between pro-fibrotic and anti-fibrotic cytokines is essential for developing targeted interventions aimed at managing chronic conditions effectively.
Cellular Changes In Fibrotic Disease
Significant cellular transformations occur during the progression of fibrotic disease, with myofibroblasts playing a central role. These specialized cells differentiate from activated fibroblasts and are marked by the expression of α-smooth muscle actin (α-SMA). Myofibroblasts contribute to excessive extracellular matrix (ECM) deposition and distort normal tissue structure in response to injury.
The activation of myofibroblasts triggers chronic inflammation and sustained tissue remodeling, impairing organ function.
Key aspects of myofibroblast activity include:.
- Secretion of collagen and other ECM components that lead to tissue stiffness.
- Promotion of inflammatory processes that exacerbate initial tissue damage.
- Alteration of tissue architecture, resulting in impaired organ functionality.
Investigating these cellular changes is vital for innovating therapeutic approaches that target fibrosis mechanisms. Such strategies could potentially reverse or slow the progression of fibrosis, ultimately improving patient outcomes in the management of fibrotic diseases.
Cytokines and Fibrosis
- TGF-β is a key driver of fibrosis, promoting the transformation of fibroblasts into myofibroblasts.
- IL-10 serves as a counterbalance to TGF-β, helping to mitigate fibrotic processes and inflammation.
- Myofibroblasts are characterized by the expression of α-SMA and are crucial in ECM deposition and tissue remodeling.
- Targeting cytokine pathways may provide new therapeutic avenues for managing fibrotic diseases.
The Connection Between Inflammation And Tissue Repair
Inflammation plays a significant role in the body’s repair mechanisms following injury or infection. This complex process is characterized by increased blood flow and heightened immune cell activity.
During this healing phase, a variety of cytokines and growth factors are released to facilitate tissue regeneration and wound healing.
When inflammation persists, the balance may tip towards fibrosis, a condition marked by excessive collagen deposition and tissue remodeling.
This unchecked remodeling can lead to diminished organ function, as observed in diseases such as pulmonary fibrosis. The interplay of inflammation and fibrosis is crucial in developing effective treatment strategies aimed at promoting healing while minimizing the risk of fibrosis development.
Chronic Conditions And Fibrosis Development
Chronic conditions are often linked with ongoing fibrosis progression.
A notable example is chronic liver disease, particularly chronic hepatitis, which frequently results in liver fibrosis as inflammation remains persistent. Chronic obstructive pulmonary disease (COPD) and idiopathic pulmonary fibrosis (IPF) are other conditions wherein inflammation significantly alters lung tissue architecture.
Pathways Linking Chronic Conditions to Fibrosis
In these diseases, pro-inflammatory cytokines, especially TGF-β, play a pivotal role in promoting collagen synthesis, fostering tissue scarring.
The interaction between inflammatory mediators and cellular mechanisms, particularly those involving fibroblasts and myofibroblasts, underscores the complexity of fibrotic alterations.
Chronic inflammation can ultimately lead to irreversible tissue damage, perpetuating a cycle of fibrosis.
Addressing these pathways is essential for effective management strategies and improving patient outcomes.
Chronic Inflammation Solutions
Addressing chronic inflammation is essential for restoring health and preventing further complications. Here are several effective strategies:
- Lifestyle Modifications: Adopting a balanced diet and engaging in regular exercise can significantly reduce inflammation levels.
- Anti-inflammatory Diet: Focus on whole foods rich in antioxidants and omega-3 fatty acids, such as leafy greens, berries, nuts, and fatty fish.
- Physical Activity: Regular exercise helps manage weight and lowers inflammatory markers.
- Stress Management: Techniques such as meditation, yoga, and deep breathing exercises can effectively decrease inflammation.
- Health Supplements: Supplements like curcumin, omega-3 fish oil, and probiotics may support anti-inflammatory pathways.
- Avoiding Triggers: Minimizing processed foods, excessive alcohol, and tobacco can alleviate symptoms.
- Sleep Hygiene: Ensuring adequate sleep is crucial for regulating inflammation.
- Integrative Health Approaches: Combining conventional and alternative medicine can enhance treatment efficacy.
- Hydration: Keeping hydrated supports cellular health and helps in reducing inflammation.
- Regular Check-ups: Monitoring inflammatory markers through routine health check-ups can help manage underlying conditions.
Inflammation and Fibrosis
- Chronic inflammation is a key contributor to the progression of fibrosis in various diseases.
- Pro-inflammatory cytokines like TGF-β are crucial in promoting collagen synthesis and tissue scarring.
- Persistent inflammation can lead to irreversible tissue damage and a cycle of fibrosis.
- Lifestyle modifications, including diet and exercise, can significantly reduce inflammation levels.
Exploring Pulmonary Fibrosis Pathways
The intricate pathways underlying pulmonary fibrosis provide valuable insight into the disease’s progression. Chronic inflammation often acts as a precursor to fibrosis, activating various cellular and molecular mechanisms.
Inflammatory cells, especially macrophages, are pivotal, as they initiate the release of cytokines, such as TGF-β, thereby promoting fibrosis.
Subsequent activation of fibroblasts leads to excessive deposition of collagen, which significantly contributes to tissue stiffness.
This interplay between inflammation and fibrotic changes highlights the urgency for targeted interventions, potentially offering hope to individuals affected by this debilitating fibrotic disease.
Mechanisms Of Extracellular Matrix Alteration
Extracellular matrix (ECM) composition undergoes notable changes during pulmonary fibrosis. These alterations impact both tissue function and repair mechanisms.
Increased collagen production leads to ECM stiffness, disrupting normal lung function. The balance of matrix metalloproteinases (MMPs) becomes compromised, which results in impaired ECM remodeling.
Such changes contribute to:.
- Impaired gas exchange
- Difficulty in tissue repair
The cellular and molecular mechanisms driving these alterations are essential for comprehending the pathology of fibrosis. Addressing these mechanisms can lead to the development of effective therapeutic interventions aimed at restoring normal ECM composition and promoting improved lung health.
Chronic Inflammation: Solutions for Symptoms
Chronic inflammation is a prolonged response that can cause tissue damage and fibrosis, necessitating proactive measures for management. Effective solutions include:
- Lifestyle modifications such as dietary changes and physical activity to decrease inflammation levels.
- Anti-inflammatory diets rich in whole foods, antioxidants, and omega-3 fatty acids.
- Regular exercise, promoting weight management and reducing inflammatory markers.
- Stress management techniques like meditation, yoga, and deep breathing.
- Health supplements including curcumin, omega-3 fish oil, and probiotics.
- Avoidance of triggers, particularly processed foods, excessive alcohol, and smoking.
- Ensuring adequate sleep, essential for the body’s healing processes and inflammation regulation.
- Hydration, which is vital for maintaining cellular health.
- Regular health check-ups to monitor inflammatory markers and underlying conditions.
Chronic inflammation correlates with various diseases, including arthritis, heart disease, and diabetes. Therefore, personalized approaches based on individual health profiles are important for effective treatment. Individuals should educate themselves on inflammation and consult healthcare providers knowledgeable about inflammation for tailored guidance.
Pulmonary Fibrosis and Inflammation
- Chronic inflammation is linked to the activation of fibroblasts, which play a crucial role in collagen deposition in pulmonary fibrosis.
- Studies show that a diet rich in omega-3 fatty acids can significantly reduce markers of inflammation in the body.
- Regular physical activity has been shown to decrease inflammation and improve lung function in individuals with respiratory conditions.
- Research indicates that stress management techniques can lower inflammatory responses and enhance overall health outcomes.
Fibroblasts And Their Role In Fibrosis
Fibroblasts serve a significant function as they are the primary cells responsible for wound healing and tissue repair. These specialized cells exhibit heightened activity during chronic inflammation, which leads to their activation and involvement in the mechanism of fibrosis prevalent in various fibrotic diseases.
Their primary role involves the production of components of the extracellular matrix (ECM), which is crucial for sustaining tissue structure.
When fibroblast activity becomes dysregulated, it can prompt an excessive accumulation of ECM, resulting in fibrosis.
The pathogenesis of fibrosis thus reflects a complex interplay, wherein persistent inflammation serves as a catalyst for fibroblast activation.
This activation can initiate fibrotic alterations that, over time, may significantly impair tissue functionality.
Strategies To Mitigate Chronic Inflammation
Exploring effective strategies for managing chronic inflammation can lead to improved health outcomes. Implementing specific lifestyle modifications can profoundly influence inflammation levels.
Dietary Adjustments
An anti-inflammatory diet focuses on whole foods, abundant in antioxidants and omega-3 fatty acids.
This dietary approach may include:.
- Leafy greens and colored fruits
- Nuts and seeds
- Fatty fish, such as salmon
Physical Activity
Regular exercise not only assists in weight management but also reduces inflammatory markers within the body. Incorporating physical activity into daily routines can yield significant benefits in combating chronic inflammation.
Stress Management Techniques
Engaging in stress-reducing practices, including meditation, yoga, and deep breathing exercises, can significantly lower inflammation levels. These methods contribute positively to both mental and physical health.
Hydration and Sleep
Hydration is essential for maintaining cellular and molecular health and regulating inflammation. Adequate sleep supports the body’s natural healing processes.
Avoiding Known Triggers
Reducing exposure to known inflammatory triggers is vital. Consider avoiding:.
- Processed foods
- Excessive alcohol consumption
- Smoking
Supplementation
Consider taking supplements, such as curcumin, omega-3 fish oil, and probiotics, to support anti-inflammatory pathways. These supplements can enhance overall health and help manage inflammation symptoms.
Integrative Health Approaches
Adopting integrative health methods that combine conventional and alternative medicine may enhance treatment efficacy. Regular health check-ups can help monitor inflammatory markers and underlying health conditions.
By implementing these strategies, individuals can better manage chronic inflammation, thereby reducing the risk of fibrosis and related health complications.
Fibroblasts and Chronic Inflammation
- Fibroblasts are essential for wound healing, producing components of the extracellular matrix (ECM) that maintain tissue structure.
- Chronic inflammation can lead to dysregulation of fibroblast activity, resulting in excessive ECM accumulation and fibrosis.
- Implementing an anti-inflammatory diet rich in antioxidants and omega-3 fatty acids can significantly reduce inflammation levels.
- Regular physical activity and stress management techniques are proven to lower inflammatory markers and improve overall health.
Chronic Inflammation And Fatigue | Hidden Triggers Revealed
Common Chronic Inflammation Foods | Uncommon Triggers To Avoid