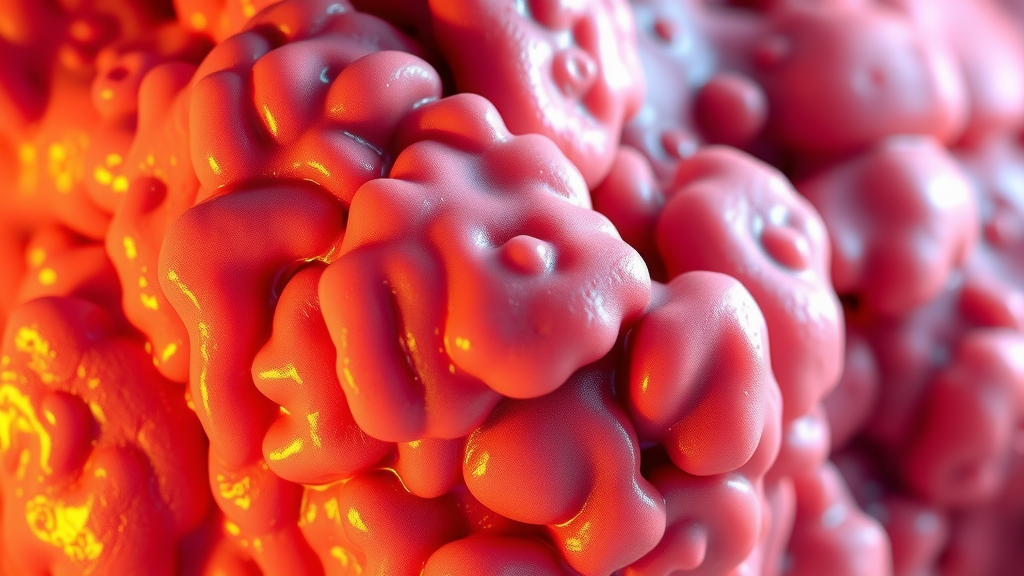
Chronic inflammation of the uterus is a condition that can significantly disrupt a woman’s health. Endometritis, a specific form of this condition, arises from various factors, including infections or irritations affecting the inner lining of the uterus.
Identifying chronic uterine inflammation is critical, as it can lead to long-lasting pelvic pain and abnormal bleeding if not addressed promptly.
Insights into endometritis can result in improved health outcomes for those affected.
‘Click here to learn more about:’ the ultimate anti inflammatory guide
Key Symptoms of Endometritis
Recognizing early symptoms plays a vital role in facilitating timely medical intervention.
Pelvic pain is a common indication of underlying endometrial inflammation, impacting daily activities. Additional symptoms may include:
- Abnormal bleeding: Irregular menstrual cycles or unexpected discharge can signal endometritis.
- Pain during intercourse: This symptom can affect relationships and emotional well-being.
- Digestive issues: Chronic uterine inflammation may sometimes lead to gastrointestinal discomfort.
Awareness of these symptoms encourages proactive medical evaluation. Early diagnosis can help avert complications such as infertility. Seeking medical advice when symptoms arise ensures appropriate treatment for endometritis, contributing to comprehensive health management.
Possible Causes of Chronic Uterine Inflammation
Several factors contribute to chronic inflammation of the uterus, including:.
- Infections: Pelvic inflammatory disease (PID) and sexually transmitted infections (STIs) like Chlamydia and Gonorrhea can lead to endometritis.
- Hormonal imbalances: Hormonal fluctuations can disrupt the menstrual cycle and promote inflammation.
- Autoimmune disorders: Conditions such as lupus can cause the body to attack its tissues, including the uterine lining.
Diagnosis and Treatment of Endometritis
Diagnosis typically involves a thorough examination, including:.
- Pelvic exams: These can help assess symptoms and detect abnormalities.
- Imaging tests: Ultrasounds or MRIs may be used to visualize uterine health.
- Laboratory evaluations: Blood tests can indicate infection or inflammation markers.
Treatment options are tailored based on the underlying cause and may include:.
- Lifestyle changes: Implementing an anti-inflammatory diet rich in omega-3 fatty acids and antioxidants can support overall health.
- Medications: Antibiotics may be prescribed to treat infections, while hormone therapy can help restore balance.
- Alternative therapies: Practices such as yoga and mindfulness can improve well-being and reduce stress, further aiding inflammation reduction.
Consulting healthcare providers to create individualized treatment plans is essential for managing chronic inflammation effectively.
Understanding Endometritis Symptoms
Awareness of endometritis symptoms is necessary for effective management. Pelvic pain can disrupt daily life and indicate a deeper issue within the reproductive system. Recognizing signs such as:
- Abnormal bleeding: Unusual menstrual patterns may require immediate medical attention.
- Fever: Elevated body temperature can suggest a serious infection requiring prompt intervention.
- Vaginal discharge: Changes in consistency or color may also point to inflammation.
Tracking these signs can help identify triggers for inflammation, facilitating timely diagnosis and treatment. Regular follow-ups with healthcare providers are vital for monitoring and adjusting treatment strategies.
Causes Of Pelvic Inflammation
Pelvic inflammation can arise from various underlying factors, forging a complex relationship between infections and chronic conditions. Infections, particularly sexually transmitted infections (STIs) like chlamydia and gonorrhea, frequently trigger pelvic inflammatory disease (PID).
These STIs can spread to the uterus, fallopian tubes, and ovaries, causing debilitating chronic inflammation.
Autoimmune disorders such as endometriosis can also incite inflammation, resulting in pelvic pain and complications.
To prevent these issues, individuals should prioritize regular screenings and adopt safe sex practices. Utilizing barrier methods, such as condoms, significantly reduces the risk of contracting infections that may lead to PID.
Chlamydia And Gonorrhea Risks
Chlamydia and gonorrhea represent significant risks to sexual health, emphasizing the need for awareness and proactive measures.
Transmission of these infections primarily occurs through sexual contact with an infected partner. Additionally, asymptomatic carriers often unknowingly spread these infections, complicating control efforts.
Untreated infections may lead to pelvic inflammatory disease, resulting in chronic pelvic pain and potential infertility in women.
Early detection through regular screenings is essential as it allows for timely treatment and minimizes complications.
Understanding the Symptoms
Symptoms associated with these infections may include abnormal vaginal discharge, pelvic pain, and fever.
Pelvic inflammatory disease caused by these STIs can also produce signs such as irregular bleeding and discomfort during intercourse. Recognizing these symptoms early prompts timely medical intervention.
Importance of Screening
Engaging in regular health check-ups assists in early detection of STIs.
Screening is particularly vital for sexually active individuals, as asymptomatic cases can lead to serious complications if left untreated. Public awareness and education about these sexually transmitted infections are necessary for effective management and prevention.
| Infection | Transmission Method | Potential Complications |
|---|---|---|
| Chlamydia | Sexual contact with infected partner | Pelvic inflammatory disease, infertility |
| Gonorrhea | Sexual contact with infected partner | Pelvic inflammatory disease, infertility |
| Pelvic Inflammatory Disease (PID) | Spread from STIs like chlamydia and gonorrhea | Chronic pelvic pain, complications in pregnancy |
Importance Of Pelvic Examination
Routine pelvic examinations are essential for the early detection of reproductive health issues. Conditions such as endometritis, characterized by chronic inflammation of the uterus, can lead to serious complications if left untreated.
Women should initiate annual pelvic exams starting at age 21; however, individual recommendations may differ based on personal risk factors.
For example, individuals with a history of pelvic inflammatory disease (PID) or a family history of reproductive issues should consider undergoing evaluations more frequently.
Recognizing symptoms like unexplained pelvic pain or abnormal bleeding is critical for seeking timely medical advice.
Regular exams enable healthcare providers to detect potential issues early, improving treatment outcomes.
Recommended Frequency of Pelvic Exams
Healthcare providers typically suggest the following frequency for pelvic exams:.
- Women aged 21 to 29: Every three years.
- Women aged 30 to 65: Every three years if they have had normal Pap tests; every five years with HPV co-testing.
- Women with risk factors: May require more frequent evaluations.
Safe Sex Practices For Prevention
Implementing safe sex practices is a fundamental step in reducing the risk of infections, particularly sexually transmitted infections (STIs). Effective preventative measures include the use of barrier methods. Condoms are one of the most reliable methods to prevent diseases such as chlamydia and gonorrhea.
Regular communication with sexual partners regarding health histories enhances mutual protection.
Effective Safe Sex Practices
- Consistently using condoms during sexual activity.
- Limiting the number of sexual partners to reduce exposure risk.
- Scheduling regular STI screenings for sexually active individuals.
- Engaging in open conversations with partners about sexual health.
Understanding Infection Risks
Fostering awareness about the implications of STIs helps individuals make informed decisions. Regular follow-up visits and consultations with healthcare professionals can further lead to better reproductive health outcomes.
Chronic Inflammation of the Uterus
Chronic inflammation of the uterus can arise from various factors, including infections, hormonal imbalances, or autoimmune disorders. Symptoms of this condition may consist of:
- Pelvic pain and discomfort.
- Abnormal menstrual cycles.
- Pain during intercourse.
Diagnosis and Treatment Options
Diagnosis often involves pelvic exams, imaging tests, and laboratory evaluations. Treatment may include:.
- Lifestyle changes such as dietary adjustments.
- Medications to manage symptoms.
- Exploring alternative therapies.
Addressing underlying causes is essential for effective management. Monitoring and adjusting treatment with healthcare professionals, including gynecologists and nutritionists, can lead to improved outcomes.
Pelvic Health
- Approximately 1 in 8 women will develop a reproductive health issue in their lifetime.
- Regular pelvic exams can reduce the risk of serious complications from conditions like endometritis.
- Using condoms can lower the risk of STIs by up to 85% when used consistently.
- Early detection through routine exams can significantly improve treatment success rates for reproductive health issues.
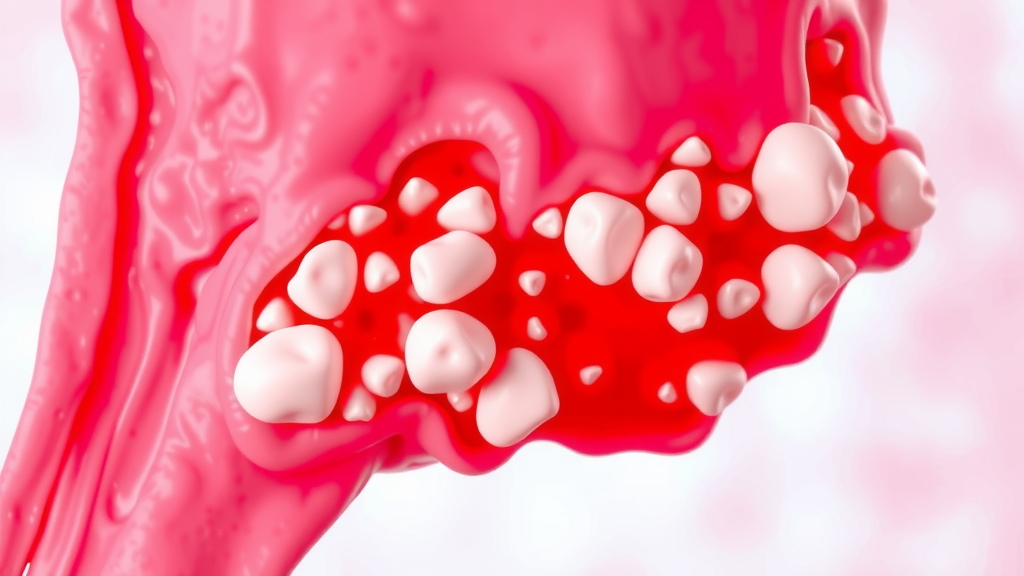
Diagnostic Approaches To Endometrial Inflammation
Accurate diagnostic methods are essential for addressing endometritis, often indicative of underlying health conditions. Clinical evaluation typically begins with a detailed medical history and a thorough pelvic examination to identify common symptoms such as abnormal bleeding and pelvic pain.
Imaging techniques, including ultrasound and MRI, are integral for visualizing the endometrium and detecting any abnormalities that may arise.
Laboratory tests, particularly endometrial biopsies, play a pivotal role in confirming diagnoses by analyzing tissue samples for signs of inflammation or infection.
Accurate diagnosis significantly aids in preventing complications associated with chronic inflammation, such as infertility and persistent discomfort.
Antibiotic Treatment Options For Infections
Effective management of endometrial infections relies on appropriate antibiotic treatment. Commonly prescribed antibiotics such as doxycycline and metronidazole effectively target prevalent bacterial infections.
Antibiotic resistance poses a growing concern, making it necessary to tailor therapy based on culture results to ensure efficacy.
Patients should remain informed about potential side effects including nausea and yeast infections.
Considerations for Usage and Monitoring
Consultation with healthcare providers for guidance on antibiotic usage and monitoring any adverse effects is crucial. This ensures successful treatment outcomes while minimizing risks associated with antibiotic resistance.
Addressing Underlying Conditions
Chronic inflammation of the uterus often results from various factors such as infections, hormonal imbalances, or autoimmune disorders.
Symptoms may include pelvic discomfort, irregular menstrual cycles, and pain during intercourse.
Diagnostic Methods
Diagnosis of chronic inflammation generally involves pelvic exams, imaging tests, and laboratory evaluations.
Tracking menstrual cycles and symptoms can help identify triggers for inflammation.
Treatment Options
Management strategies can include lifestyle changes, such as adopting an anti-inflammatory diet and engaging in regular exercise to alleviate symptoms.
Mind-body practices, including yoga and meditation, may also support overall well-being and reduce inflammation. Consulting healthcare professionals like gynecologists and nutritionists can provide tailored treatment plans.
Natural supplements such as turmeric and ginger are noted for their anti-inflammatory properties and may aid in managing chronic inflammation of the uterus.
Regular follow-ups with healthcare providers are vital for monitoring symptoms and adjusting treatment strategies to ensure optimal uterine health.
Endometrial Health
- Endometritis can lead to serious complications, including infertility, if not diagnosed and treated promptly.
- Antibiotic resistance is a significant issue, necessitating the use of culture results to guide effective treatment.
- Lifestyle changes, such as diet and exercise, can significantly impact the management of chronic uterine inflammation.
- Natural supplements like turmeric and ginger are recognized for their anti-inflammatory effects and may assist in reducing symptoms.
The Role Of White Blood Cells
White blood cells (WBCs) serve as key defenders in the body’s immune system. These cells, including neutrophils and lymphocytes, perform vital functions by identifying and targeting pathogens such as bacteria and viruses.
Neutrophils are often the first responders to infections, quickly mobilizing to initiate a defensive response against invaders.
Lymphocytes, on the other hand, are tasked with producing antibodies, which provide protection against future infections.
Maintaining a healthy balance of WBCs is essential; for instance, high levels may indicate an ongoing infection or inflammation, while low levels can signify immune deficiencies, raising the risk for conditions like endometritis and chronic inflammatory diseases.
Impacts On Fertility And Childbirth
Chronic infections can have a profound effect on reproductive health, potentially hindering fertility. Chronic inflammation of the uterus, frequently resulting from infections such as pelvic inflammatory disease (PID) or endometriosis, can lead to scarring and persistently cause pelvic pain, thereby complicating conception efforts.
Untreated infections contribute to heightened risks of complications during pregnancy, including miscarriages and preterm labor. To address these risks, early diagnosis through pelvic examinations and timely interventions like antibiotic treatments are critical.
Engaging in a healthy lifestyle—including regular screenings, stress management, and a balanced diet—can promote reproductive health and overall wellness.
Chronic Uterine Inflammation
Chronic inflammation of the uterus can manifest as prolonged irritation and swelling, resulting in symptoms such as pelvic pain, abnormal bleeding, and digestive issues.
Common causes include:.
- Infections like PID
- Hormonal imbalances
- Autoimmune disorders
Diagnosis typically involves pelvic exams, imaging tests, and laboratory evaluations. Recommended treatment options may include:
- Lifestyle changes, including dietary adjustments
- Medications to manage symptoms
- Alternative therapies complementing traditional treatments
Addressing underlying causes, such as infections or hormonal irregularities, is crucial for effective management. Potential lifestyle adjustments include:.
- Incorporating an anti-inflammatory diet, rich in omega-3 fatty acids and antioxidants
- Regular exercise to improve blood flow and reduce stress
- Practicing mind-body techniques like yoga and meditation for overall wellness
Consulting healthcare professionals, including gynecologists and nutritionists, can lead to tailored treatment plans. Tracking menstrual cycles can help identify triggers related to inflammation. Maintaining a healthy weight and managing stress are also vital for hormonal balance. Some natural supplements, such as turmeric and ginger, possess anti-inflammatory properties. Seeking early intervention may prevent complications associated with chronic inflammation, and regular follow-ups with healthcare providers are essential for monitoring and modifying treatment strategies.
White Blood Cells and Reproductive Health
- Neutrophils account for 50-70% of all white blood cells and are essential for the body’s initial defense against infections.
- Chronic pelvic inflammatory disease (PID) affects approximately 1 million women in the U. S. each year and can lead to long-term reproductive health issues.
- Studies suggest that maintaining a balanced diet and regular exercise can significantly improve reproductive health and reduce inflammation.
- Early diagnosis and treatment of infections can decrease the risk of complications during pregnancy, including miscarriage rates by up to 50%.
Chronic Condition Management Strategies
Effectively managing chronic inflammation of the uterus requires a multifaceted approach tailored to individual needs. Personalized treatment plans must consider specific symptoms and underlying causes to ensure optimal care.
Chronic inflammation may arise from infections, hormonal imbalances, or autoimmune disorders, requiring a comprehensive strategy that integrates both medical and lifestyle interventions.
Implementing lifestyle changes plays a significant role in managing this condition.
Adopting an anti-inflammatory diet can greatly reduce inflammation.
Foods rich in omega-3 fatty acids, such as fatty fish, wild-caught salmon, and walnuts, are especially beneficial. Incorporating antioxidants through fruits and vegetables can also aid in reducing inflammation.
Regular exercise promotes blood circulation and helps alleviate stress, contributing positively to overall health.
Integrating medical advice with these lifestyle modifications is essential in crafting a cohesive management strategy. Treatment options can include lifestyle changes, medications, and alternative therapies, with a clear focus on addressing underlying causes to enhance overall uterine health.
When To Seek Medical Attention
Being aware of symptoms that necessitate timely medical intervention is critical in managing chronic inflammation.
Severe pelvic pain that persists or worsens might indicate complications requiring immediate medical evaluation.
These complications may involve conditions such as endometritis or other infections that necessitate prompt care.
Additionally, persistent abnormal bleeding or unusual vaginal discharge can signal underlying issues needing further investigation.
Symptoms such as fever or chills may also suggest a potential infection, underscoring the importance of seeking medical advice swiftly. Ignoring these signs can lead to serious complications, highlighting why awareness of symptoms is vital for maintaining reproductive health.
Recognizing the importance of timely intervention can greatly improve treatment outcomes and quality of life.
Chronic Condition Management
- Research indicates that an anti-inflammatory diet can significantly reduce markers of inflammation in the body.
- Regular exercise is shown to improve blood circulation and lower stress levels, both of which are beneficial for managing chronic inflammation.
- Timely medical intervention for symptoms like severe pelvic pain can prevent complications such as endometritis.
- Persistent abnormal bleeding or unusual vaginal discharge are critical symptoms that warrant immediate medical evaluation to rule out serious conditions.
Prevention Magazine Chronic Inflammation | 5 Surprising Ways To Reduce Inflammation
Why Do I Have Chronic Inflammation? | Unique Relief Stories For Chronic Inflammation